By continuing your visit to this site, you accept the use of cookies.
Learn + I agreeLearn more
Transmission mode of zoonoses
The diseases transmitted by animals are called zoonoses. The majority of them are due to emerging pathogens that used to be rare but are becoming more frequent. This increase in zoonoses is due to increase in outdoor activities (hiking in the mountains or forest) and the increased number of pets and types of pets.
We regroup under the term zoonosis all diseases that can be directly transmitted from animals to humans as well as diseases indirectly transmitted through a vector such as ticks or mosquitoes.
The types of direct and indirect transmission for zoonotic diseases vary greatly :
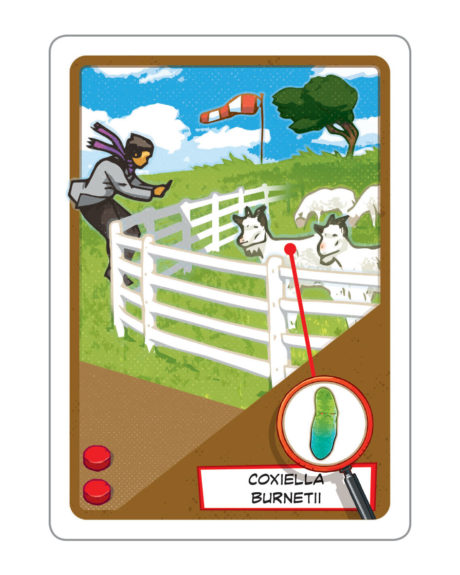
- Some bacteria (as for example Coxiella burnetii or Chlamydia psittaci) can directly be transmitted through air.
Coxiella burnetii is very resistant to drying out and can be transported over long distance by the wind. It was shown that in southern France the cases of Q fever were increased when there was a high wind activity from the north (mistral) (1,2).
A small epidemic of Q fever that affected 14 people happened in Lavaux in 2012. This epidemic was due to an infected flock of sheep (1200 total) that released infectious air. As a first protective measure the flock was moved to an unpopulated area (lake Hongrin). If you want to know more about this Q fever epidemic I recommend the paper published by C. Bellini et al. (3).
- In 2007, a small epidemic of psittacosis appeared in an aviary located in a public park in Lausanne (Switzerland). A local daily reported it and, thanks to this newspaper article, an attentive doctor suspected a C. psittaci infection in his neighbor who complained of flu-like symptoms (4). C. psittaci has also been detected in wild pigeon populations in cities (5). In addition, several cases of psittacosis have been recently observed in Australia following contacts of veterinarians with sick horses (6).

- Other pathogens are transmitted through cat (Pasteurella) or rat (Leptospira) bites or cat scratches (Bartonella).

-
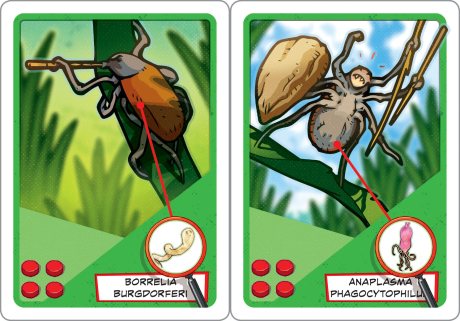
In addition, a vast repertoire of bacteria are indirectly transmitted to humans by arthropods. Well known examples are spotted fever group rickettsia, Borrelia burgdorferi (Lyme disease), Francisella tularensis, Ehrlichia, Babesia,Anaplasma and others.
- Fleas mainly transmit the bacteria Bartonella henselae (cat scratch disease agent), Rickettsia typhi (endemic typhus agent) et Yersinia pestis (plague agent). The first type of flea lives on cats while the other two reside on rodents.
- Body lice (Pediculus humanus humanus) can transmit three species of bacteria Rickettsia prowazekii (epidemic typhus agent), Bartonella quintana (trench fever agent ) and Borrelia recurrentis (relapsing fever agent). The latter one shows the importance of classifying bacteria at the species levels as it belongs to the same genus (Borrelia) as the Lyme disease causing Borrelia burgdorferi.
Other zoonotic diseases
Besides the four pathogens transmitted by animals described in the game KROBS (Bartonella henselae, Coxiella burnetii, Pasteurella multocida and Chlamydia psittaci), there is a whole array of other zoonotic diseases. Here you can find a brief overview of the most important ones :
- Plague is caused by Yersinia pestis a bacteria discovered in 1894 by Alexandre Yersin, a famous swiss microbiologist. The bacteria goes from the rat to humans through fleas. There is a very contagious and rapidly fatal pulmonary form as well as a bubonic one (high fever and swollen lymph nodes).
- Rat-bite fever is an infection by Streptobacillus moniliformis. This disease causes a fever, headaches, and joint inflammation and sometimes more severe cardiac or renal complications that can be fatal.

- Leptospirosis is caused by bacteria of the genus Leptospira that are found in the urine of infected animals such as wild rodents, dogs or livestock that then contaminates the ground and water. Sewage drainer workers, fish and rice farmers and veterinarians are at high risk of exposure. There is also a risk when doing outdoor activities in water such as canoeing, fishing or swimming. Leptospirosis is due to a bacteria related to Borrelia burgdorferi that belongs to the spirochetes group. It can manifest with flu-like symptoms, fever, headache, joints and muscle pain or in a more severe form reaching multiple organs such as the liver and kidneys.

- Rabies is due to a virus (rhabdovirus) and is transmitted by bites (mainly dogs). Bats can also transmit the disease. Even in absence of documented rabies cases in the region a person that has been bitten by a bat should consider herself at risk of exposure. The rabies virus causes encephalitis that is almost always fatal once the symptoms have appeared. There is a preventive vaccine and a therapeutic vaccine that can be used, but only prior to symptoms appearance.

- Tularemia is a disease that affects the lymph nodes and is caused by the bacteria Francisella tularensis. It is mainly transmitted by ticks, but can sometimes be acquired through scratches or bites with an infected mammal (small rodent).
- Ehrlichiosis affect white blood cells and other blood cells. They are caused by different bacterial species such as Ehrlichia chaffeensis and Anaplasma phagocytophilum and are transmitted by tick bites. The symptoms resemble the flu, but can sometimes lead to chronic severe forms.
- Rickettsioses are mainly transmitted by tick bites for the spotted fever group and by rat fleas for the typhus group (Rickettsia typhi).
Tick-transmitted rickettsioses cause spotted fevers characterized by an encephalitis, a black mark where the bite occurred and a rash.

There are many different types of spotted fever which are dependent on the type of ticks found in a specific region. For example, Rickettsia conorii causes Mediterranean spotted fever and is transmitted by the tick Rhipicephalus sanguineus that can only be found in the Mediterranean region. First cases were described in Tunisia in 1909 by A. Conor that named the species.
Tick-borne lymphadenitis is a disease caused by Rickettsia slovaca that is found throughout Europe as members of the tick genus Dermacentor are present on the whole continent. Dermacentor have a preference for hair and therefore the black mark is often not visible.
Clinical manifestations of rickettsioses are also affected by the tick feeding behavior. Ticks of the genus Amblyomma that can sense the CO2 emitted by mammals (zebras, antelopes and humans that visit the national parks of South Africa and Swaziland) can be infected by Rickettsia africae the infectious agent of African spotted fever. This disease is characterized by occurrence in grouped cases and multiple black marks on the same individual. This is due to the feeding behavior of Amblyomma ticks that attack in groups the same person.
- Brucellosis is also known as undulant fever, Malta fever and Mediterranean fever.
Brucelloses are due to different bacterial species Brucella melitensis, Brucella abortus and Brucella suis. Brucella melitensis is transmitted to humans by dogs, sheep, and camels, Brucella abortus by cattle, camels and buffalos, and Brucella suis by pigs and caribous. Brucella causes miscarriages in most infected animals and is usually suspected by the veterinarian faced with this situation. Diagnosis can be confirmed on aborted material by culture, microscopy or PCR.

People in close contact with animals are at higher risk of exposure (farmers, butcher, slaughter house workers, or veterinarian), but bacteria can also be transmitted through the consumption of raw milk and derived products as well as aerosols.
Brucellosis causes a fever and a variety of symptoms depending on the infected organs, such as endocarditis, arthritis, etc..
- Anthrax is a zoonotic disease that used to kill entire flocks before a vaccine became available. This disease is still endemic in some African countries where animal vaccination is not enforced. The infectious agent is Bacillus anthracis, a germ that can form spores that can survive in the soil for many years. Before the work of Robert Koch on B. anthracis anthrax epidemics among livestock were frequent as dead animals were buried in the pasturing fields causing the disease to reoccur.

This practice led to the belief of « damned fields ». The spores if B. anthracis would stay for years dormant in the soil and be transported back through worms to new animals.
Anthrax presents in three forms : cutaneous (low risk in 80% of cases), gastrointestinal (rare but mortal in 25-60% of cases depending on treatment delay) and the most severe respiratory (90-100% mortality in absence of care and 50% with antibiotics). Humans can be infected by inhaling spores (respiratory form), getting spores in cuts (cutaneous form) or eating contaminated meat (gastrointestinal form).
Classification of zoonoses
Zoonoses can be classified as follows :
- According to the transmitting animal
For example cats can transmit toxoplasmosis, cat scratch disease, pasteurellosis while dogs transmit rabies, toxocariasis or leishmaniosis.
Cattle transmit listeriosis, Tenia saginata and brucellosis and sheep mainly transmit Q fever and brucellosis.
Rats transmit rat-bite fever and tularemia while birds are the vectors for psittacosis and avian flu.
And finally arthropod-vectors such as ticks and fleas transmit borreliosis, tularemia, rickettsioses and ehrlichioses as well as plague.
- According to the type of causal agent
We distinguish between diseases caused by bacteria (rickettsioses, brucellosis, Q fever, leptospirosis, Lyme disease, psittacosis, tularemia,…) and viral diseases (Lassa fever, avian flu, rabies,…).
There are also zoonotic diseases caused by parasites (leishmaniosis, toxoplasmosis) and fungi (ringworm).
- By transmission mode
There are essentially three modes of zoonotic transmission:
(i) through aerosols (Q fever, psittacosis, brucellosis, anthrax),
(ii) by inoculation: bites (leptospirosis, pasteurellosis, rabies, tularemia) or scratches (bartonellosis, …),
(iii) through arthropod-vector bites: ticks (rickettsioses, ehrlichioses, tularemia, borreliosis, tick-borne encephalitis) , fleas (bartonellosis, plague, endemic typhus) or lice (epidemic typhus, trench fever, recurrent fever, …).
References
- Tissot Dupont H, Amadei MA, Nezri M, Raoult D. Wind in November, Q fever in December. Emerg Infect Dis. 2004 Jul;10(7):1264-9.
- Tissot-Dupont H, Torres S, Nezri M, Raoult D. Hyperendemic focus of Q fever related to sheep and wind. Am J Epidemiol. 1999 Jul 1;150(1):67-74.
- Bellini C, Magouras I, Chapuis-Taillard C3, Clerc O, Masserey E, Peduto G, Péter O, Schaerrer S, Schuepbach G, Greub G. Q fever outbreak in the terraced vineyards of Lavaux, Switzerland. New Microbes New Infect. 2014 Jul;2(4):93-9.
- Senn L, Greub G. Local newspaper as a diagnostic aid for psittacosis: a case report. Clin Infect Dis. 2008 Jun 15;46(12):1931-2
- Geigenfeind I, Vanrompay D, Haag-Wackernagel D. Prevalence of Chlamydia psittaci in the feral pigeon population of Basel, Switzerland. J Med Microbiol. 2012 Feb;61(Pt 2):261-5.
- Polkinghorne A , Greub G. A new equine and zoonotic threat emerges from an old avian pathogen, Chlamydia psittaci. Clin Microb Infect. 2017 Oct; 23 (10): 693-4.
Learn more by other websites
Zoonosis (in french): https://www.bag.admin.ch/bag/fr/home/krankheiten/krankheiten-im-ueberblick/zoonosen.html
